Welcome to Can We’s conversation on cervical screening and cervical cancer prevention
Did you know that LGBTQ people are less likely to have cervical screening than the general population? Everybody with a cervix is at risk of cervical cancer. If you have a cervix, you need to screen. It’s that simple. 15 minutes every 5 years could save your life. Can We is here to help our communities stay healthy.
It's Your Cervical Screening Test - Own It
ACON's Cervical Screening campaign, Own It, empowers all women and people with a cervix to own their Cervical Screening Test. Own It provides information about choices you have when it comes to your Cervical Screening Test. Here you’ll find everything you need to know about cervical screening, including HPV and the Cervical Screening Test, how to book your test and the choice of testing options available. If you have questions, Can We is here to answer them.
Can We talk about cervical cancer and screening?
what is cervical cancer?
Cervical cancer is the growth of abnormal cells in the lining of the cervix, the lowest part of the uterus or womb. Most cervical cancers are caused by the human papillomavirus (HPV).
Cervical cancer develops slowly, taking an average of 10-15 years from an HPV infection. That’s why cervical screening is so important, and why testing for HPV is effective in detecting potential problems much earlier so that they can be monitored or treated to prevent cervical cancer from developing.
What is the Cervical Screening Test?
The Cervical Screening Test is how we screen for cervical cell changes so that they can be monitored or treated to prevent cancer from developing. It’s for anyone with a cervix who has ever been sexually active—regardless of gender identity, sexuality or sexual history. Cervical cancer doesn’t discriminate.
The test looks for HPV (human papillomavirus). If your test is positive, meaning HPV was found, your sample is tested for any cervical cell changes. Your doctor will advise you if anything is detected and if you need further tests or treatment.
If your test is negative, meaning no HPV found, you come back in five years for your next Cervical Screening Test. You’re eligible for your first test at 25. Screening occurs until age 74.
How to do a self-collection Cervical Screening Test
Everybody attending for a Cervical Screening Test can chose if they would like their clinician to collect their sample or if they would like to collect their own sample. This is called self-collection.
Self-collection involves a vaginal / front hole swab. The collection device looks like a long cotton bud. You insert the swab into your vagina/front hole up to the red line and rotate for 30 seconds (see below diagram), then you put the swab back in its tube and hand it over to be tested.
Self-collected Cervical Screening Test:
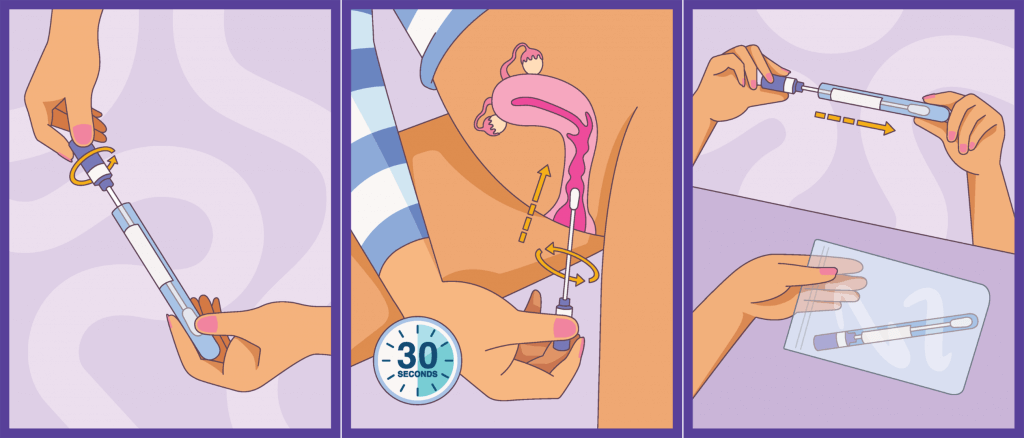
(credit: www.health.gov.au/initiatives-and-programs/national-cervical-screening-program)
The clinician collected and self-collection samples are the same in terms of picking up the presence of HPV variants that cause most cervical cancers.
If your test comes back positive for HPV, you’ll be referred for further testing to look to see if there are any changes in the cells of your cervix, which may need monitoring or treatment to prevent cervical cancer from developing.
To find out when you’re next due for a Cervical Screening Test, call the National Cancer Screening Register on 1800 627 701.
Clinician collected Cervical Screening Test:
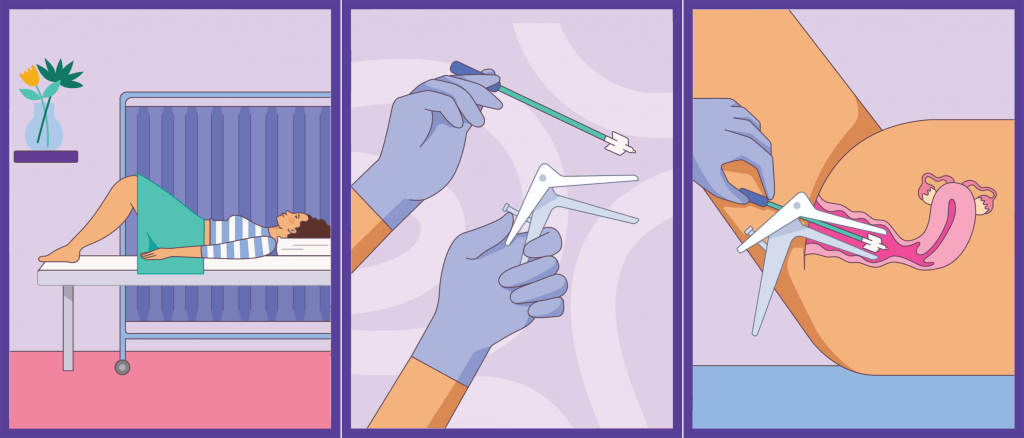
(credit: www.health.gov.au/initiatives-and-programs/national-cervical-screening-program)
Who needs to screen?
If you have a cervix, you’re at risk of cervical cancer
If you have a cervix and you’ve ever been sexually active, you need to have regular cervical screening. It does not matter if you’re gay, lesbian, bisexual, trans or queer. If you’ve had the HPV vaccination or not. Whether you’ve only had one partner, or if you no longer have sex. If you’ve been through menopause, or don’t have penetrative sex. If you’ve had a partial hysterectomy. Even if you have a cervix, but a doctor says that you don’t need to screen. There are so many myths out there and Can We is here to bust them. Everybody with a cervix is at risk of cervical cancer. If you have a cervix and you’ve ever been sexually active, you need regular cervical screening from the age of 25.
Visit In The Know to find out more about screening for breast and bowel cancer as well as cervical cancer.
THE CERVICAL SCREENING TEST PROCESS
The test collects a sample of cells during an internal exam, typically taking a few minutes.
Self-Collected Cervical Screening Test
Your doctor or nurse will explain how to collect your sample. You’ll be given a swab, you’ll head somewhere private (like behind a medical screen or bathroom) and you insert the swab a few centimetres into your vagina / front hole. Once you’re done, you put the swab back in its tube and hand it back to the doctor or nurse who will send it to the lab to be tested.
This collection method aims to give people more control over their Cervical Screening Test whilst making it more comfortable and less invasive.
Clinician Collected Cervical Screening Test
The process involves undressing from the waist down and lying on your back or sitting up a little with your knees bent on an exam table.
Your healthcare provider will insert a speculum and use a small brush to take the sample from the cervix. You can also insert the speculum yourself, which is more comfortable for some people.
With either collection method, the sample of cells will go to a lab and be tested for HPV. If you test positive for HPV, your doctor will advise you about the next steps which may require further testing or treatment.
If you test negative for HPV, then you come back in 5 years for your next Cervical Screening Test. Check out the video below to learn more.
What actually happens during a Cervical Screening Test?
Check out this video to learn what happens during a Cervical Screening Test.
Can I do the test myself?
Check out this video if you want to know more about self-collection.
I'm trans, do I need to screen?
Do trans men and trans masc folk with a cervix need cervical screening?
Yes. Trans men who have a cervix and are 25 years of age or older are at risk of cervical cancer and need regular cervical screening.
What if I’m on testosterone?
Being on testosterone doesn’t reduce your risk of developing cervical cancer. For some people on testosterone (and some post-menopausal people), hormonal changes to the front hole/vagina can make getting a good sample from the cervix difficult and uncomfortable. A prescription from your GP for topical oestrogen before your test can help make it more comfortable – it’s only temporary and rarely has side effects. Alternatively, you can opt to self-collect your sample if you prefer.
I’ve had a hysterectomy. Do I still need cervical screening?
If you’ve had a partial hysterectomy, which preserves the cervix, you need to continue cervical screening. If you’ve had a full hysterectomy (where your uterus was entirely removed including the cervix), you don’t require cervical screening. To be certain talk to your doctor to check if you need to continue cervical screening or not.
People who don’t have a cervix are still able to get a test that is similar to the Cervical Screening Test (in that it can test for the presence of HPV and look for any changes to the cells of the vagina/front hole). Talk to your doctor about whether you need to continue having the test, it will depend on your medical history before you had the hysterectomy.
My Medicare gender is ‘male’ and I have a cervix – will I be added to the Register?
If you’ve had a Pap or Cervical Screening Test at any point in your life, you will have been added to the Register automatically, even if your gender is male under Medicare.
The National Cancer Screening Register gets information from Medicare, so if you need to change your personal details, it has to be done through Medicare. You can call on 132 011, check your Medicare account here, or use your MyGov account to change your details.
If you have never had a Pap or a Cervical Screening Test, you have changed your Medicare gender to male, and you still have a cervix, you will not be automatically added to the National Register (the Register only automatically adds people whose gender is ‘female’ under Medicare). If you’re under 25, talk to your GP or healthcare provider about getting a reminder letter when your turn 25 (some medical centres and GPs will do reminder letters for Cervical Screening). As soon as you’ve had your first test, you will be added to the Register and receive reminders. If you’re over 25, book your screen here.
Do trans women need to screen?
There isn’t a lot of research on trans women and cervical screening, but the risk of developing “cancer of the neo-vagina” (as it’s known in medical terminology) for trans women or other people who have had vaginoplasty is thought to be very low. The risk of cancer developing from HPV will depend on what type of surgery you have had as well as your personal health history (things like previous HPV infections, HIV or auto-immune conditions). Talk to your doctor about your personal risk factors. Visit TransHub to find a gender-affirming doctor.
What if I don’t have a cervix, should I get tested for HPV?
Some people have vaginas but don’t have a cervix. This can include some trans women, some trans men, some intersex people and people who’ve had full hysterectomies. They are able to get a test that is similar to the Cervical Screening Test (in that it can test for the presence of HPV and look for any changes to the cells of the vagina/front hole).
HPV testing for people who weren't born with a cervix isn’t usually covered by Medicare and isn’t part of a standard STI test. If you’re really worried, talk to your doctor about the pros and cons of HPV testing.
If you’ve had a full hysterectomy (meaning you used to have a cervix and don’t anymore), talk to your doctor about whether you need to continue to have the test – it will depend on your medical history before you had the hysterectomy.
How can we stay healthy?
Why is cervical screening so important for Aboriginal and Torres Strait Islander people?
Aboriginal people are 2.5 times more likely to get cervical cancer than the rest of the population. While the Cervical Screening Test is effective for preventing cancer, participation in cervical screening among Aboriginal and Torres Strait Islander people is low. It’s so important to get regular screening tests.
You can go to these places for a Cervical Screening Test:
• your doctor/GP
• an Aboriginal Health Service
• some women's and community health centres
• Well Women's Clinics and Services at hospitals
Ask your doctor, nurse or Aboriginal health worker when and how you can get the test and your results. Remember, that self-collection is now available and that most Cervical Screening Test results are normal, but you need to have the test to make sure.